During the 1840's in Vienna there was a problem that everyone knew about but no one seemed to be able to solve. The problem was that a lot of mothers died after giving birth from an illness called "childbed fever". In the 1840's no one knew what caused this illness that claimed so many young lives - mothers and new borns - and devastated so many families. Without a cause an effective treatment was elusive.
The worst part of this problem was that the people of Vienna knew that mothers were much more likely to die of childbed fever if they were looked after by the doctors than by the nurses. Mothers often took desperate measures to avoid going into hospital on the days when the doctors were on call!
In 1846 a young Hungarian doctor called Ignaz Semmelweis (1818 - 1865) started work at Vienna General Hospital and quickly became aware of the childbed fever problem because part of his job was to keep the obstetric clinic records. Semmelweis realised that there was a problem that none of his medical training provided an answer for and for the next six months he searched for an explanation and a solution.
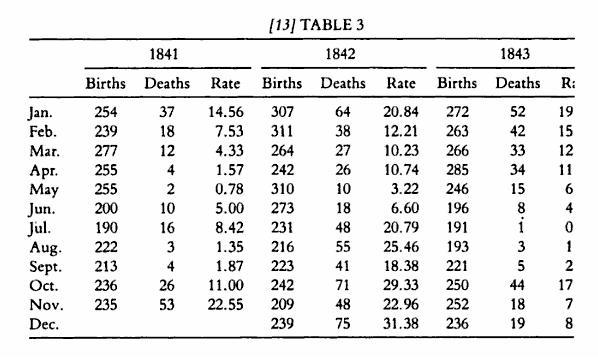 The image shows part of a table of mortality data presented by Semmelweis in the book he published in 1861.
The image shows part of a table of mortality data presented by Semmelweis in the book he published in 1861.
In 1842 on the doctors wards there were 3067 births and 521 deaths - an average mortality of 17% - with a peak in December 1842 of 31%!
The clue that led to the breakthrough was a chance observation in 1846 - when one of his colleagues accidentally cut his finger while conducting a post-mortem and subsequently died of an illness that looked very like childbed fever.
Along with other clues this led Semmelweis to the idea that something was being transferred from the dead bodies in the morgue to the live patients on the ward and this "something" was the cause of the childbed fever and the cause of the deaths of both mothers and babies.
It was a radical and shocking idea that the doctors themselves might be the unwitting carriers of some unknown agent that caused such a tragic disease! The concept also suggested a possible solution - to ensure that doctors washed their hands in a solution of chlorine before entering the maternity ward. In May 1847 this solution was tested when Semmelweis implemented routine hand-washing using chloride of lime - and enforced its use vigorously.
To download the BaseLine© Case Report of Semmelweis's work and its historical context click here
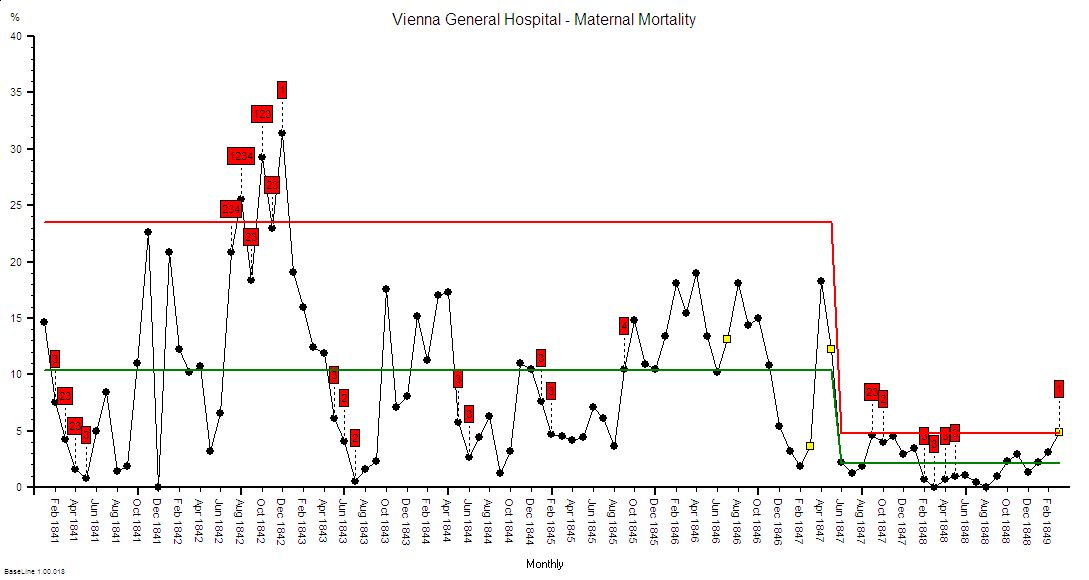
The process behaviour chart above has been created using BaseLine© using the data published by Semmelweis - who never presented the data in this format. It shows the maternal mortality data from the First Clinic at Vienna General Hospital for the period Jan 1841 to Apr 1849. Prior to the introduction of hand-washing the maternal mortality was, on average, over 10% - with a peak in Dec 1842 of over 30%; that is one-in-three previously healthy mothers died shortly after childbirth! The chart shows clearly that 1842 was a particularly bad year; and it also shows that in the summer of 1843 the mortality rate fell to almost zero. On the face of it the data supported the accepted view that childbed fever was an epidemic illness caused by uncontrollable external factors - but to Semmelweis this hypothesis did not explain why the mortality on the Second Clinic was an average of 2% - and this ward was run by nurses. What was different between the two wards that were next to each other in the same hospital? The possible transmission of an unknown agent from the morgue on the hands of the doctors was a radical idea but one that fitted the facts.
The immediate and dramatic impact of hand-washing on maternal deaths on the First Clinic is very obvious from the chart - the average mortality dropped to match that of the Second Clinic and the wide variation from month to month also reduced. This "accident of fate" was in retrospect the first strong evidence that the deaths were caused by an unknown agent and this insight helped in the development of the Germ Theory by Robert Koch in Germany and Louis Pasteur in France. Germ theory led to the rational use of a different antiseptic by Joseph Lister in Scotland and it was not until 1879 that Louis Pasteur demonstrated streptococci in the blood of women with childbed fever - over thirty years after Semmelweis's original discovery.
The story is a timely reminder that what we can't see often causes us greater problems than what we can - and that blindness is as much perceptual as actual. Semmelweis was unable to convince his peers - they did not see what he did in the evidence.
The fate that befell Ignaz Semmelweis was not as favourable as his innovation - he was clearly aware that he had unwittingly been the cause of many deaths because, prior to 1847, like his peers he performed many post mortems and with the same contaminated hands then examined the women on the labour ward. After he had discovered a practical solution but not an explanation he was unable to convince his peers who did not immediately accept his interpretation without proof of the mechanism. Rather than publishing his data and looking for the causal agent he wrote critical letters to the leaders of the medical profession at that time, accusing them of murder. This counter-productive behaviour only increased resistance to his ideas and effectively condemned many more women to an early death. It is interesting to note that it was his students who spread the message more effectively than he did! An important lesson to all innovators - the way in which a message is conveyed is as important as the message itself.
Semmelweis left Vienna in 1849 when his two year contract finished and was not renewed. He subsequently worked in several other obstetric wards where he introduced his hand-washing technique and saw similar improvements. In desperation Semmelweis eventually published his work in 1861 but his book was very critical of other influential doctors across Europe. His behaviour became progressively unacceptable and he was eventually incarcerated in a lunatic asylum and is believed to have died from septicaemia caused by infection of injuries that he sustained their at the hands of his carers. A somewhat ironic end - to be locked up as a madman and die from the very disease he was trying to save the world from!
With the benefit of hindsight we can learn two important lessons from this true story:
1. When the evidence of what actually happens does not fit with what we predict will happen then one possibility we must always consider is that our understanding may be incorrect. We may be wrong. Only by entertaining this possibility do we have an opportunity to improve our understanding.
2. It is almost impossible for us to accept a change to a new way of doing things without a rational explanation of how the new method is better and the reasons why. Better still, if we can also experience the benefit with our own sense as we are naturally distrustful of the opinion of others - just as they are often distrustful of ours.
3. Presenting objective measurements in the form of process behaviour charts can help us with both of these challenges; firstly in diagnostic mode we are able to highlight the special causes and seek an explanation for them; and in prognostic mode we are able to test our predictions against reality and learn from the outcome.
Footnote
To download the BaseLine Case Report of Semmelweis's work and it's historical context click here
